Dietary Approaches for Irritable Bowel Syndrome

Irritable bowel syndrome is a common, often intractable problem that causes abdominal pain and diarrhea, constipation or both. Standard approaches often focus on fiber and using compounds that affect gut motility, the rhythmic contractions that move food through the gastrointestinal tract. While in some cases these compounds can decrease symptoms, they aren’t a cure.
More recently, research into food triggers and dietary approaches has started to gain significant attention and traction. Dairy is well known to cause symptoms in a percentage of patients with gastrointestinal problems (Vazquez 2020). Wheat and gluten are often triggers as well, even outside of celiac disease (Roszkowska 2019). The sugar fructose also appears to commonly play a role (Ikechi 2017). All of these components involve difficult to digest sugars, including lactose, fructans and fructose.
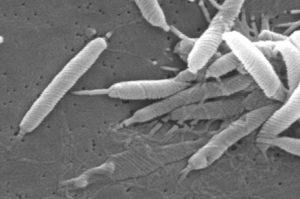
One of the newer theories of the cause of irritable bowel syndrome is based around the idea of an overgrowth of bacteria in the small intestine (SIBO) or problematic flora in the colon (Pimentel 2016). These bacteria consume indigestible or hard to digest sugars which creates gastrointestinal symptoms from bacterial metabolites. The hard to digest sugars also increase water influx into the digestive tract which can cause loose stools.
The Low FODMAP diet
Diets aimed at eliminating these hard to digest sugars are low FODMAP diets. FODMAP stands for a diet low in fermentable, oligosaccharides, disaccharides, monosaccharides, and polyols. While different variations of the diet exist, they generally all work to significantly reduce difficult to digest sugars.
The latest research suggests significant benefits for irritable bowel in following a low FODMAP diet. A meta-analysis of studies showed a reduction in pain and bloating for IBS (Altobelli 2017). However, long-term data on low FODMAP diets is still lacking. The diet itself is quite restrictive and patients often find it challenging. In addition, there are concerns for meeting all of your nutritional needs when following the diet.
When implementing a low FODMAP diet, it’s recommended to work with a knowledgeable provider. The diet contains two phases. The first phase is much stricter, where most high FODMAP foods are eliminated. After 4-8 weeks, if symptoms improve, the second phase is implemented where individual foods that contain FODMAPs can be reintroduced to see what provides the most expansive diet and still maintains symptom relief.
Low Sucrose and Starch Diet
A separate but similar dietary approach looked at reducing sugar (sucrose) and starch. Individuals struggling with IBS that followed a low sugar and starch diet had significant improvement. Within four weeks, one-third of patients no longer qualified for a diagnosis of IBS with two-thirds of patients having significant improvement in symptoms (Nilholm 2019).
The diet stemmed from the discovery of an increased prevalence of patients that can’t digest sucrose and isomaltose in IBS (Nilholm 2019). These individuals had genetic variants for enzymes that don’t break down these sugars effectively in the gastrointestinal tract.
Processed Foods

There also appears to be a link between “ultra-processed foods” and irritable bowel syndrome. Individuals with the highest consumption of ultra processed foods had a 25% higher risk for having irritable bowel syndrome (Schnabel 2018).
Decreasing processed foods in the diet is another strategy that can help reduce symptoms. Examples of ultra-processed foods include confectionery, biscuits, cakes, ice cream, sweetened beverages, sweetened dairy products, mass-produced packaged breads, prepared meals, poultry and fish nuggets, hot dogs and other reconstituted meat products, brick soups, breakfast cereals and artificial sweeteners.
Conclusions
Evidence is starting to build that dietary factors other than fiber may play a role in irritable bowel syndrome. Exploring dietary triggers, especially with a knowledgeable healthcare provider, may provide insight into ways of eating that can help control symptoms. Considering the prevalence of IBS, having additional, effective tools to help with treatment is definitely welcome.