Osteoporosis Prevention and Treatment: Diet and Nutrients
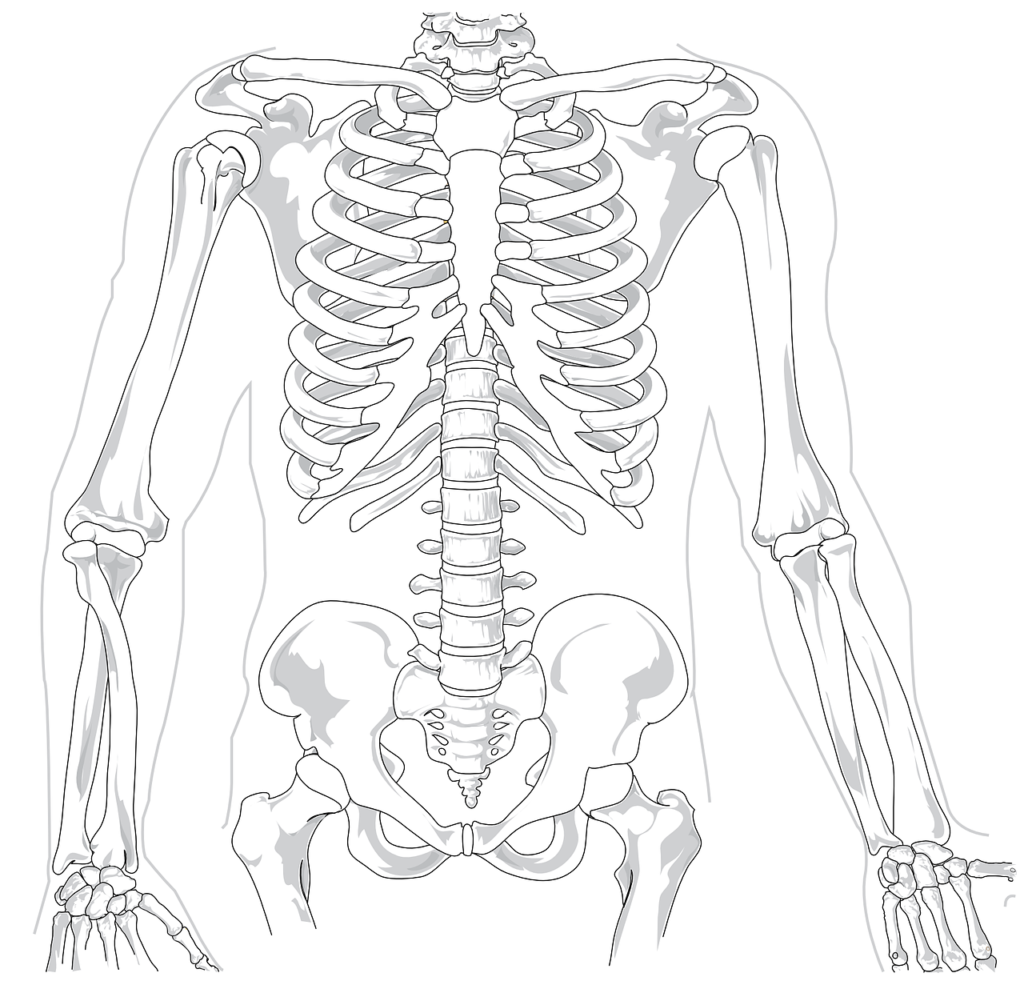
As we get older, bone loss can lead to increased fracture risk. This weakening of the bones, if severe enough, is called osteoporosis. Hip fractures in the elderly often lead to serious consequences. One study showed that 33% of elderly individuals died within one year of an osteoporotic hip fracture (Guzon-Illescas 2019). Bone loss is typically a gradual process that is influenced by dietary and lifestyle behaviors. With that being said, it’s possible to help prevent and even reverse some aspects of osteoporosis with some natural approaches.
Some of the potential treatments for preventing and reversing osteoporosis can include proper diet and supportive nutrients.
Eating to Prevent Osteoporosis
Diet is an important part of preventing osteoporosis. While more data is needed, evidence suggests that dietary factors may help decrease or prevent fractures.
Protein
Eating too much protein was once thought to be a cause of osteoporosis (Bonjour 2013). Proteins are composed of amino acids. Researchers had concerns for bone calcium loss due to the need to buffer the amino acids associated with excess protein consumption. It was initially thought that eating less protein might help prevent osteoporosis. While most people think of calcium when they think of bones, bones also contain significant phosphorus and magnesium. In addition, half the volume of bone is composed of protein (Munoz-Garach 2020).
The latest research suggests higher protein diets are protective for bone. Eating more than the minimum recommended daily protein requirements is associated with higher levels of bone density, slower rates of bone loss and decreased risk for hip fractures (Rizzoli 2018). Interestingly, vegan diets, which are often lower in protein, are associated with higher risks of bone loss (Ho-Pham 2009).
The Mediterranean Diet

The Mediterranean diet probably has the strongest evidence for decreasing the risks of bone loss and fractures. The diet typically focuses on vegetables, whole grains, beans, nuts and seeds with fruit as a typical dessert. Meat is still a component of the diet, although red meat is generally consumed approximately once per week (Martin-Pelaez 2020). A meta-analysis showed a 21% reduction in the risk of hip fracture with a Mediterranea diet (Malmir 2018).
Foods rich in polyphenols also appear to provide protection. Darker colored fruits and vegetables, olive oil, beans and tea can be rich sources of polyphenolic compounds (Chisari 2019). While we aren’t completely sure why polyphenols provide benefits, it may be due to their anti-inflammatory characteristics. Keeping your diet high in fruit and vegetables, beans, olive oil and tea will likely help keep your bones healthy.
Dairy Products
And finally, it’s worth mentioning the research around dairy products. Long-touted as the most important food group to build strong bones, the research support of dairy and bone health is decidedly mixed. A study out of Sweden showed high milk intake associated with higher fracture risk in older women (Michaelsson 2014). A meta-analysis of the data found no relationship between milk consumption and fracture risk (Bischoff-Ferrari 2011). A further study evaluating the data on higher dairy consumption found that dairy products in general are not protective for bone fractures (Willett 2020). From the published data, I don’t recommend eating larger quantities of dairy products to prevent bone loss.
Minerals
Calcium
The alkaline minerals, calcium, magnesium and potassium, all potentially play a role in building bone and protecting from osteoporosis, although the data is somewhat complex. Calcium, long thought to be key for maintaining bone health, doesn’t show strong results for protecting from osteoporosis in the trials published so far. While it does appear to have consistent effects in increasing bone mineral density and slowing loss, benefits are modest (Wu 2017). Some analyses have also found no benefit in elderly individuals with calcium supplementation for fracture prevention (Zhao 2017). While calcium is vital during childhood and teen-age years, on its own, it doesn’t appear to provide robust protection from bone loss in the elderly.
There’s also emerging evidence that calcium supplementation on it’s own may increase risks of heart disease, although calcium from food had no associated risks (Yang 2020). While I still will recommend calcium at times, it’s important to use better absorbed forms (not calcium carbonate) and to take calcium with magnesium. While not proven, magnesium may help prevent the heart disease risks of calcium supplementation.
Magnesium
As mentioned previously, bones are composed of more than just calcium, they also contain magnesium and phosphorus. Magnesium intake appears to play a role in bone health, with analyses suggesting that magnesium from diet increases bone mineral density and that low blood levels of magnesium correlate with osteoporosis (Farsinejad-Mars 2016, Zheng 2014). In the short term, supplementing with magnesium decreases bone turnover (Aydin 2010). Long-term supplementation was shown to increase bone mineral density modestly and potentially prevent age-related bone loss (Sojka 1995).
Potassium
Emerging research on potassium is also starting to suggest that it can prevent bone loss. A trial of over 200 elderly men and women given potassium bicarbonate were found to significantly reduce markers of bone loss over the six month trial (Dawson-Hughes 2015). Additional research on potassium citrate appears to suggest similar results (Gregory 2015). A longer study on potassium citrate showed bone building effects after two years of supplementation (Jehle 2013). Potassium is not a major constituent of bone, it likely protects bone health by buffering acidity. When potassium is available in large supply, the body doesn’t need to use calcium as a buffering agent, preserving bone structure.
Trace Minerals
Other research suggests trace minerals may enhance calcium’s effects on bone. A study on calcium with zinc, copper and manganese found the combination worked better than calcium alone (Strause 1994). It’s likely other nutrients enhance the benefits of supplemental calcium as well.
Boron
Boron is a trace mineral with a number of interesting actions on the body including antimicrobial, anti-inflammatory and hormone balancing effects. There’s even early evidence appearing to indicate protection of the brain and central nervous system that may have implications for dementia (Khaliq 2018).
Additional research is starting to suggest that boron also has effects on bone health. In animal studies, boron appears to support bone mineralization and regeneration (Hakki 2010, Uysal 2009). There’s also some preliminary evidence that boron improves bone density (Volpe 1993). In mice deficient in boron, bone remodeling is inhibited, showing the necessity of the nutrient for bone health (Gorustovich 2008).
Vitamin D
Recently, recommendations around bone health and vitamin D have been controversial. A spate of meta-analyses on vitamin D and bone fracture prevention (as a symptom of osteoporosis) showed little to no benefit. However, numerous problems with the analyses and other published data still suggest that vitamin D prevents fractures in at-risk elderly individuals, especially if they have a vitamin D deficiency (Bischoff-Ferari 2019). More well done trials are needed to fully understand vitamin D’s benefits for osteoporosis. If you are deficient in vitamin D, you will likely benefit from supplementation. It’s best to get tested to assess your levels.
Vitamin K
Vitamin K is primarily known for supporting the blood clotting cascade. Older blood thinners work by inhibiting its activity. It’s a common misconception that taking too much vitamin K can cause blood clots—it can’t. Vitamin K is only involved in the normal clotting process and excess does not cause increased clotting risks (Asakura 2001).
While a number of trials seem to suggest vitamin K can help with osteoporosis prevention, many of these studies suffer from significant bias (Mott 2019). Evidence does suggest that it might decrease fractures, however study authors caution that more evidence is needed to confirm the results. The form of vitamin K may also be important, but again, more studies are needed to flesh out the best use of vitamin K for bone health.
Conclusions
Dietary factors and several nutrients appear important for preventing and treating bone loss and osteoporosis. With how common, and how problematic, fractures can be in the elderly, dietary and nutritional strategies for preventing osteoporosis could provide some significant benefits.