Stomach Ulcers, Mental Health and Treating Helicobacter pylori
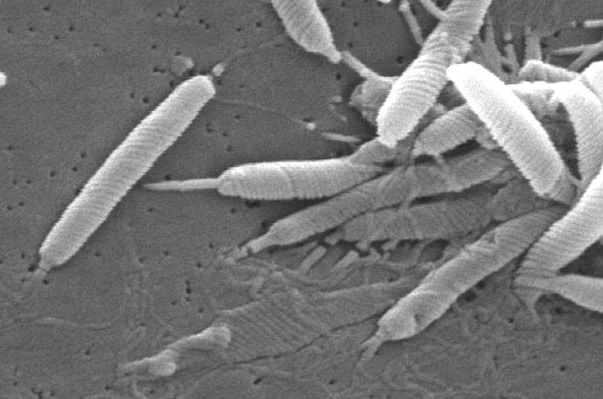
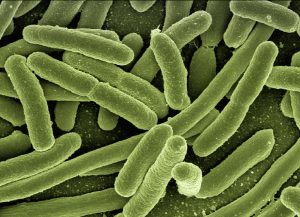
Last week’s article discussed how infection with the bacteria that causes stomach ulcers, Helicobacter pylori, appears to affect mental health. For patients who are infected and have symptoms, eradication of the bacteria is recommended. Unfortunately, standard treatment for H. pylori is typically fairly aggressive, using three or four drugs for two weeks. Even with four drugs, resistance is not uncommon and varies by region around the world (Rokkas 2021).
In addition, I have personal concerns over H. pylori treatment regimens. Over my career, I have seen multiple patients who have developed long-standing irritable-bowel-type symptoms after receiving H. pylori treatment. Antibiotics do not discriminate, and using multiple antibiotics for up to two weeks can cause significant damage to the healthy intestinal flora that can be difficult to reverse. As such, it’s worth seeing if any natural or integrative treatment options have enough research on efficacy and safety to consider them as an alternative approach.
Why Treating H. pylori Is Challenging: A Hypothesis
While I know of no research on this, I suspect that H. pylori is difficult to treat because of its location in the stomach. Standard antibiotics come as capsules or tablets. When a capsule or tablet is swallowed, it starts to dissolve in the stomach, but can quickly move into the small intestine. Since H. pylori is in the stomach, once the antibiotic has passed into the small intestine, it is likely no longer effective. It’s hard to imagine that an antibiotic will be absorbed into the body, circulate through the blood back to the stomach and travel through the stomach lining to kill the bacteria. Antibiotics probably have one chance to kill H. pylori during their initial pass through the stomach. Liquid formulations may, therefore, coat the stomach better, leading to improved treatment efficacy.
Again, this is only a hypothesis on my part, as there is no evidence I could find supporting my assumptions, but it may be worth keeping in mind for treatment.
Natural H. pylori Treatments
Raw Green Cabbage Juice
The discovery of the anti-stomach-ulcer effect of green cabbage juice traces back to research from the 1940s and 50s, before we even knew about H. pylori stomach infections. One of the first published trials used fresh cabbage juice in 13 patients with stomach ulcers (Cheney 1949). The therapy healed the ulcer within seven to ten days based on its location. Standard therapy at the time took between 37 and 42 days to heal the ulceration. A further study in 100 patients by the same author found complete pain relief in 86% of patients who had stomach ulcers with similar rapid healing of the ulceration as compared to standard treatments (Cheney 1952).
A contrary study on 24 hospitalized patients compared cabbage juice to standard therapy and found no difference between the two (Doll 1954). Bed rest combined with an anti-ulcer diet was compared to the same treatment with added cabbage juice. The author’s suggest their patients may have been different somehow, or they weren’t using the right type of cabbage. Other studies from Italy and Russia exist on the efficacy of cabbage juice, but were unavailable for translation and review.
More recent animal studies also suggest that cabbage may be a viable treatment for H. pylori and stomach ulcers (Hadda 2014, Carvalho 2011). Sulforaphane, a compound found in numerous cruciferous vegetables, including cabbage, also appears to inhibit H. pylori (Johansson 2008).
Licorice Root (Glycyrrhiza glabra)

As an herb, licorice root has a long history of use in both Chinese and European herbal medicine. While licorice candy nowadays is often made with anise, historically, the sweet taste of licorice root was typically the flavoring. As an herbal treatment, licorice root was often used to treat gastrointestinal conditions. And the root itself shows some antibacterial properties with potential efficacy against H. pylori (Asha 2013).
Clinical trials are few, but suggest promise. One study combined licorice with standard antimicrobial therapy versus standard therapy alone (Hajiaghamohammadi 2016). Elimination of H. pylori was 83% with the combined treatment, whereas standard medications were only 63% effective. A trial combining licorice root extract and a probiotic-fermented milk also showed reduced levels of H. pylori with improved gastrointestinal symptoms (Yoon 2019). It’s likely the treatment dose was too low to fully clear H. pylori as they only used 100 mg of licorice extract administered just once daily.
A separate trial used quadruple drug therapy either with bismuth (the standard medication) or with licorice extract (Momeni 2014). In the licorice group, H. pylori eradication was 67% as compared to 57% with the standard therapy.
A trial of licorice root extract alone versus placebo also showed significant results (Puram 2013). Licorice root extract was taken daily for one month. At the two month follow up, 48% of the patients who had taken licorice root were clear of H. pylori as compared to 2% of patients on placebo.
As an herb, licorice root should be utilized with caution. Taking too much licorice for too long can cause elevations in blood pressure by reducing potassium levels.
Blackseed (Nigella sativa)
Another herb that appears to hold promise in the treatment of H. pylori is blackseed or black cumin. The herb has been compared to standard triple therapy for H. pylori, and while not as effective, it still worked surprisingly well as a treatment (Salem 2010). In the study, standard therapy was effective in 83% of patients, whereas 2 grams a day of blackseed combined with an acid blocking medication was 67% effective.
A more recent study combined ground blackseed with standard triple therapy as compared to triple therapy alone (Naini 2020). The combination treatment was more effective, clearing H. pylori 88% of the time as compared to just 55% with standard therapy. In a separate study, honey and ground blackseed was taken three times a day after meals for two weeks (Dabaghian 2016). For those patients that completed the regimen, 57% were cleared of the H. pylori infection.
While blackseed oil if often used medicinally, it may have less of a potent effect on H. pylori (Esmail 2019). A study that used blackseed oil with a stomach acid blocker only cleared H. pylori infections in 30% of children.
Probiotics
And finally, probiotics also appear to have an impact on helping to clear H. pylori infections while decreasing side effects when combined with other treatments. A meta-analysis of the research found that higher dose probiotics with mixed strains of bacteria were more effective for H. pylori than lower doses (Musazaheh 2023).
Conclusion
H. pylori infections in the stomach can be resistant to standard treatment. A number of natural approaches appear to hold promise, including cabbage juice, licorice root, blackseed and probiotics. With additional research, we can hopefully develop protocols that are safer and have fewer side effects than standard treatments.